
- Personality Psychopathology & Impulse-Control Disorders
- Personality psychopathology
- A personality disorder is characterized by:
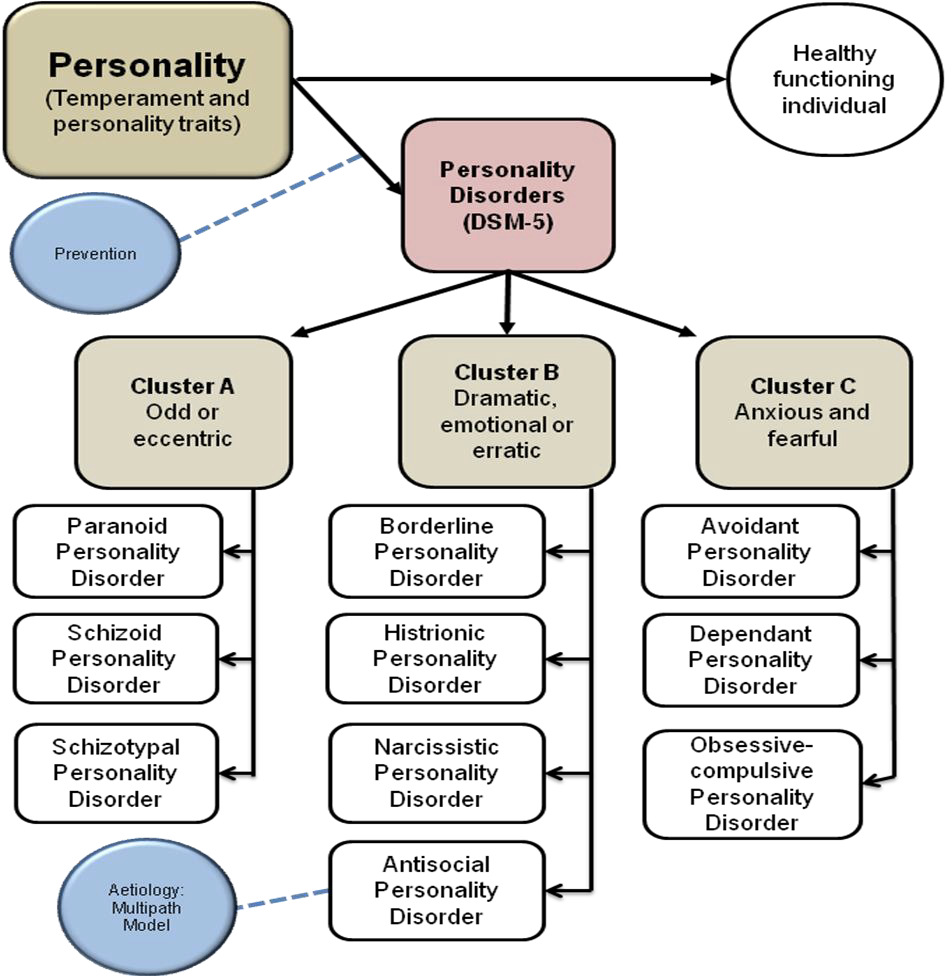
- Diagnostic and Classification methods
- Categories
- Paranoid personality disorder
- Schizoid Personality Disorder
- Schizotypal Personality disorder
- Antisocial Personality Disorder (APD)
- Borderline Personality Disorder BPD
- Histrionic Personality Disorder
- Narcissistic Personality Disorder
- Avoidant personality disorder
- Dependent personality disorder
- Obsessive -Compulsive Personality Disorder
- Impulse control Disorders
- Looking at antisocial personality disorder with the multipath model
- Issues with diagnosis
- Disorders of childhood and adolescence
Personality Psychopathology & Impulse-Control Disorders
This assignment covers:
- Personality psychopathology chapter 14
- Disorders of childhood and adolescence Chapter 15
- About 30 pages of the study guide, from page 58 Tut letter 501
Personality psychopathology
Dysfunctional and maladaptive personality patterns that are long term and present in nearly all situations
Personality Disorder
When maladaptive personality characteristics are problematic for the person and others, then the person may be diagnosed with a personality disorder.
A personality disorder is characterized by:
- impairment of self and interpersonal functioning
- pathological personality traits that are long-standing and relatively inflexible
- Personality patterns involve behavior, thoughts, emotions and interpersonal functioning
- Criteria for diagnosis:
- The patterns are longstanding.
- These patterns are extreme and deviate from cultural expectations
- They are inflexible and pervasive across situations
- They are evident from adolescence or early adulthood and stable over time
- They are associated with distress and impairment.
People with a personality disorder often function well enough to be independent and successful, and may not see themselves as having a problem.
They often do not seek help. So the incidence of personality disorders is uncertain. There may be a lifetime prevalence of 9 to 13%. About 5-15% of people who receive professional help have personality disorders.
Diagnostic and Classification methods
- Categorical diagnostic model: 10 personality disorder categories representing 10 clinical syndromes
- Alternative model: both dimensional and categorical assessment
Categories
The 10 personality disorders are grouped into 3 clusters:
- Odd/eccentric behaviors:
- Paranoid (mistrust & suspicion)
- schizoid (isolated, cold, indifferent to others)
- Schizotypal (peculiar thoughts & behaviors, poor interpersonal relationships)
- Dramatic, emotional & erratic behaviors
- Antisocial (not conforming to social codes, lack of anxiety & guilt, irresponsible behaviors)
- Borderline (intense fluctuations in mood, self image & interpersonal relationships)
- Histrionic (sef-dramatisation, exaggerated emotional expression, seductive/provocative/attentions seeing behaviors)
- Narcissistic (exaggerated sense of self importance, exploitative behavior, lack of empathy)
- anxious/fearful behaviors
- Avoidant (Social inhibition, fear of rejection and humiliation)
- Dependent (excessive dependence on others, inability to assume responsibilities, submissive)
- Obsessive-compulsive (perfectionist, controlling interpersonal behavior, devotion to details, rigidity)
Paranoid personality disorder
“A pervasive distrust and suspiciousness of others such that their motives are interpreted as malevolent.”
- suspiciousness, hypersensitivity, reluctance to trust others
- Expectation that others will mistreat or exploit them
- Tend to be rigid in their thinking and preoccupied with unfounded beliefs eg: My wife is cheating on me.
- May seem aloof and lacking in emotion
- Often interpret other people’s behavior negatively, question their loyalty and bear grudges
- Paranoid beliefs are very resistant to change
- socially isolated and usually fail to seek treatment
- Prevalence: 2.3 to 4.4%
- Somewhat more common in males

Schizoid Personality Disorder
“Pervasive detachment from social relationships and a restricted range of emotions in interpersonal settings”
- Social isolation, emotional coldness and indifference to others
- Do not desire or enjoy close relationships
- Often live alone
- Solitary hobbies
- Withdrawn & reclusive
- Perceived by others as peculiar and aloof
- Relationships are superficial and frequently awkward
- Prevalence 3.1 to 4.9% in the US
- somewhat more common in males

Schizotypal Personality disorder
- Odd, eccentric, paranoid and peculiar thoughts and behaviors
- a high degree of discomfort with and reduced capacity for interpersonal relationships
- Many believe they possess magical abilities or special powers
- some are subject to recurrent illusions
- Often have speech oddities such as frequent elaboration, digression or vagueness in conversation
- Social anxiety
- Up to 3.9% prevalence in US. Slightly more males than females

Antisocial Personality Disorder (APD)
“A pervasive pattern of disregard for and violation of the rights of others”
- Diagnosis only applies from the age of 18 and older.
- Chronic antisocial behavioral patterns such as a failure to conform to social or legal codes
- lack of anxiety or guilt
- irresponsible behaviors
- Little concern for wrongdoing,
- lying, using people, perpetuating aggressive sexual acts

- Superficial and fleeting relationships with others with little loyalty
- Seek power over others
- Often manipulate, deceive, exploit and con others for their own needs and purposes.
- Includes the terms psychopath and sociopath, especially for those with a pattern of emotional detachment, low levels of anxiety or fear, a bold interpersonal style and high levels of attention seeking.
- Prevalence in the US 0.4 – 4.5%.
- Many more males than females
Antisocial personality disorder is different from impulse control disorder, being part of a criminal subculture or civil disobedience
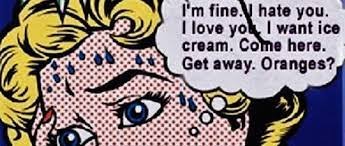
Borderline Personality Disorder BPD
- Volatile emotional reactions
- instability in interpersonal relationships
- Poor self image
- Impulsive responding
- Lack a strong sense of self-identity and have a fragile self-concept that is easily disrupted by stress

- Intense fluctuations in mood
- intense hypersensitivity to social threat
- volatile interactions with friends, family and even strangers
- Chronic feelings of emptiness
- Form unstable and intense social relationships
- May indulge in binge eating, substance abuse, self-injury, verbal aggression and impulse shopping
- may fluctuate between being friendly and hostile
- Many people with BPD have suicidal behavior – well above average -often triggered by interpersonal conflicts and events
- Sexual difficulties are also common
- Occasionally people with BPD may have psychotic symptoms such as auditory hallucinations, usually transient and recognised by the person as not based in reality.
- Some correlation with a traumatic and difficult childhood as well as affect lability in the brain
- Prevalence in the US is 1.6 to 5.9
- Up to 10% of people with BPD die by suicide
- Long term remission is possible & DBT is a specific technique developed for working with BPD.
- DBT (Dialectic behavioral therapy) addresses:
- suicidal behaviors
- behaviors that interfere with therapy
- Behaviors that interfere with quality of life
- reactive behaviors
- post traumatic stress behavior
- self-respect behaviors
- DBT (Dialectic behavioral therapy) addresses:
- More women than men

Histrionic Personality Disorder
“Pervasive pattern of excessive emotionality and attention-seeking”
- histrionic = intensely dramatic emotions and behaviors
- self-dramatization
- exaggerated expressions of emotions
- attention seeking behavior
- so possibly flamboyant and flirtatious behavior
- superficiale warmth and charm, but shallow and self-centered.
- US prevalence 0.4 – 1.8%
- Gender differences are not found, but more women present in a clinical setting

Narcissistic Personality Disorder
“A pervasive pattern of grandiosity, need for admiration, and lack of empathy.”
- sense of entitlement
- exaggerated self-importance
- superiority
- Desire for constant attention and approval
- difficulty accepting criticism
- Overestimate their own talents and importance
- Some people are capable of empathy, but others not
- US prevalence 0 – 6.2%
- Treatment is difficult and focussed on helping clients:
- develop empathy for others
- understand the needs of others
- decrease self-involvement

Avoidant personality disorder
“a pervasive pattern of social inhibition, feelings of inadequacy and hypersensitive to negative evaluation”
- fear of rejection and humiliation make the person reluctance to initiate social relationships.
- negative sense of self, low self esteem & strong sense of inadequacy
- avoid social situations and relationships
- often socially inept, shy &withdrawn
- fear humiliation, overly sensitive to criticism, blame themselves for things that go wrong
- may take little pleasure in life
- May feel inferior, inadequate, depressed or anxious
- crave affection and social contact
- US Prevalence 1.4 – 5.2%, no gender differences
May be on a continuum with social anxiety disorder, or it may be distinct disorder that includes social anxiety.
May be caused by an interaction between childhood environment and innate temperament.
Hypersensitivity to rejection may trigger a positive feedback loop.
Clients with avoidant personal disorder may be reluctant to confide about themselves during therapy, so building rapport and a therapeutic alliance is essential.
Research shows that CBT can be effective in treatment.

Dependent personality disorder
“A pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fear of separation.”
- dependency and inability to take responsibility
- resulting in depression, helplessness and suppressed anger.
- Lack self-confidence and subordinate their needs to the people they depend on.
- May seem understanding and tolerant
- May tolerate dominance and abuse for fear of their partner leaving
- US prevalence is 0.5%, and gender differences are still unclear.
Research shows that dependency is associated with overprotective or authoritarian parenting.
Cognitive theorists address core assumptions:
- The person may believe they are inherently inadequate and unable to cope.
- They then believe they need someone to take care of them.

Obsessive -Compulsive Personality Disorder
“Pervasive pattern of preoccupation with orderliness, perfectionism and mental and interpersonal control at the expense of flexibility, openness and efficiency.”
- Preoccupation with details and rules
- Inability to see the big picture
- focus on being control of one’s life and emotions
- Focus on minor details
- Need to control other people
- Lack flexibility
- Rigid behavior which can impair their occupational and social functioning.
- Others may find people with OCOD to be demanding, inflexible and perfectionistic
OCPD is different to OCD (obsessive compulsive disorder). People with OCD have unwanted intrusive thoughts and or urges that are distressing, whereas OCPD is a personality issue, which is seen by the person who has the disorder as preferable and correct.
Impulse control Disorders

- Intermittent explosive disorder:
- periodic aggressive episodes which may result in injury or damage
- impulsive aggressiveness that is out of proportion to the situation
- Are not generally aggressive between episodes and may feel genuine remorse for their actions
- Kleptomania
- fail to resist the impulse to steal
- Are not stealing out of need
- Feel irresistible urges and tension that is relieved by stealing
- Pyromania
- Urge to set fires
- Fascinated by and get intense pleasure from setting fires or watching them burn or be put out
- the desire to set fires is driven by this urge rather than by practical motives such as vengeance etc.
Looking at antisocial personality disorder with the multipath model
I am not going to go into this in depth. The textbook gives some interesting reading on the biological, social, psychological and sociocultural causes for antisocial personality disorder, and how they may interact. Moving on….
Issues with diagnosis
The problem with the categorical diagnostic method, which is being used above is that it is:
- unreliable – the disorders overlap, so different clinicians will give different diagnoses
- high comorbidities may mask the personality disorder eg Post traumatic stress disorder PTSD may mask Borderline personality disorder BPD.
- The reality is a continuum. We can all recognize at least some of the traits in each category in ourselves. The categories are all or none.
For these reasons, a dimensional model is very useful.
It allows for a continuum, and looks at:
- personality functioning:
- identity
- self direction
- empathy
- intimacy, etc
- and specific traits:
- social withdrawal
- affect
- antagonism
- psychoticism
This alternative model removes 4 of the personality disorder categories: paranoid, schizoid, histrionic & dependent, and uses both the categories and the diagnostic model according to clinician preference.
Disorders of childhood and adolescence

Very different measures of what is normal and healthy and what is psychopathological to those in adulthood.
The prefrontal cortex is associated with attention, self control and being able to take perspective. It is only fully mature in early adulthood, so children think and behave quite differently to adults, and think and behave quite differently as they grow up.
However childhood mental disorders have a similar prevalence to in adults – about 50% in the US.
The most common of these is anxiety.
Internalizing disorders
These are disorders with emotional symptoms that are directed inwards
- heightened reactions to trauma, stressors and negative events
- difficulty tolerating distress
- difficulty regulating emotions
- the most common internalizing disorders are anxiety and depression
- These are risk factors for suicide and substance abuse.
- When young people show abrupt changes in behavior, self-destructive and/or sexualized behavior, there may be a need for assessment to rule out sexual abuse.
Anxiety, traumas, stressor-related disorders

Anxiety, trauma and stressor related disorders are usually from a combination of biological predisposition and environmental issues.
The most common anxiety disorders are phobias (starting early – mid childhood) and social phobia (starting early to mid-adolescence).
- extreme worry
- discomfort
- fear of unfamiliar and anxiety provoking situations
- can lead to adult anxiety disorders
- children who are inhibited and fearful are at greater risk.
- Parental styles that increase risk:
- overprotective and controlling parents
- low parental warmth
- perceived parental rejection
- Separation anxiety disorder: fear of leaving home, being separated from caregiver or being along
- Selective mutism: Failure to speak in some situations
Attachment disorders
When children and babies grow up in stressful unpredictable home environments, they may battle to form attachments and social relationships.

- Reactive attachment disorder: inhibited, and not seeking or responding to comfort, attention or nurturing. Watchful and avoidant. Rarely show positive emotions and may demonstrate:
- irritability
- sadness
- fear
- Disinhibited social engagement disorder: Socialize effortlessly but indiscriminately, attaching themselves to strangers and acquaintances, and moving away from caregivers.
- these children often have a history or harsh punishment and inconsistent parenting as well as emotional neglect and limited attachment opportunities.
- When children start to get predictable and nurturing care, Reactive attachment disorder often disappears. Disinihibited social engagement disorder is more persistent.
Post Traumatic Stress Disorder PTSD

- Youth with PTSD experience recurrent distressing memories
- triggered by threats of or direct experience with death, serious injury or sexual violation
- Memories may entail:
- nightmares
- intense physiological and or psychological reactions to thoughts and cues associated with the event
- episodes of playacting the event
- dissociative reaction in which the child relives the trauma or seems unaware of the present situation.
- Children may seem socially withdrawn , show few positive emotions or lose interest in activities they used to enjoy.
- angry aggressive behavior, tantrums
- difficulty sleeping or concentrating
- exaggerated startle response & vigilance
Non-suicidal self injury NSSI

- intentionally inflicted superficial wounds
- Often preceded by intense negative thoughts & emotions and thought about self-harm
- At least 5 times over a year
- Cutting etc can provide relief from painful feelings and a temporary feeling of calm and wellbeing
- Also serves as a form of self-punishment
- Associated with increased risk of attempted suicide
- negative cognitive style and negative self-talk are associated with both NSSI and with attempted suicide.
- Usually begins in early adolescence
- both genders
- Dialectic behavior therapy has been helpful
- May self-resolve over time
Mood disorders

- depressive disorders most prevalent in girls and older teenagers.
- Often caused by environmental factors in childhood
- Genetic and biological factors in adolescence
- Environmental triggers may include:
- childhood abuse (physical , mental & sexual)
- parental mental & physical illness
- loss of an attachment figure
- Strong association between depression and suicidal ideation & attempts, so treatment is a priority.
- Evidence-based treatment includes:
- CBT (individual & group)
- Family-focused therapy
- building resilience through positive psychology programs
- Selective serotonin reuptake inhibitors SSRIs are risky because they are associated with an increased risk of suicide.

Disruptive Mood Dysregulation Disorder
- chronic irritability and severe mood dysregulation including frequent tempers and anger
- Anger is intense and/or of long duration and may include verbal and physical aggression
- Outward expression of sad, depressive and unhappy mood.
- Often predict later depressive and anxiety disorders
Pediatric Bipolar disorder PBD
A serious disorder that is similar to adult bipolar disorder
- mood changes
- distinct periods of elevated energy and activity with less sleep, distractibility, talkativeness or inflated self-esteem
- May also have recurring depressive episodes or periods of irritability.
- poor prognosis
Externalizing disorders
Disruptive behavior disorders – these disorders have symptoms that are distressing to others
A persistent pattern of behavior that is atypical for the child’s developmental level and cases significant distress to the child and others, or negatively affects ability to function.

Oppositional Defiant Disorder ODD
A persistent pattern of angry, argumentative or vindictive behavior that continues for at least 6 months
- negative affect and emotional dysregulation
- defiant and oppositional behavior
- may resolve or evolve into a conduct or depressive disorder

Intermittent explosive disorder
A pervasive, persistent and seriously impairing disorder
To be diagnosed with IED, a person will have
- recurrent outbursts of extreme aggression twice weekly for at least 3 months
- or 3 outbursts within a year that result in damage or injury.
- Unpremeditated and in response to minor provocation
- The child’s mood is normal between outbursts
- The child is 6 and older
Associated with early exposure to familial aggression, violence and interpersonal trauma. May be comorbid with attention-deficit hyperactivity disorder ADHD, conduct disorder or ODD

Conduct disorder
Persistent pattern of antisocial behavior that represents dysfunction within the individual including serious violations of rules and social norms and disregard for the rights of others.
Diagnosis requires 3 or more of the following:
- deliberate aggression (bullying, fights, weapons, cruelty to people or animals, aggressive theft, sexual assault
- destruction of property, incl setting fires
- theft or deceit
- serious violation of rules
Often becomes more serious with age.
Boys with CD are more aggressive, girls are more inclined to substance abuse, truancy and lying. About half of youth with CD also have inattention and hyperactivity. About 2 – 9% of youth meet the criteria for CD.
Some youth with CD have limited prosocial emotions – minimal guilt, empathy. Manipulative, superficial affect and charm, cruelty and aggression. High risk of continuing criminal behavior and being diagnosed with antisocial personality disorder in adulthood.
Etiology of externalizing disorders eg: CD
- Often being early in childhood.
- Out of the four factors (social, psychological, sociocultural an d biological), biology seems to play the most important role in CD.
- In both CD and APD, there seem to be brain abnormalities associated with deficits in social information processing, as well as reduced activity in the amygdala (less fear than the norm)
- This results in a decreased ability to learn from rewards and punishments
- Genotype low activity MAOA (allele associated with fear-regulating circuitry in the amygdala.
- People with this genotype then get subjected to childhood maltreatment. Elevated stress hormones – cortisol – associated with impulsive aggression, and low cortisol with callous unemotionally and predatory aggression
Psychological, social and sociocultural dimensions
- Sociocultural: large family size, crowding, male gender, poverty
- Psychological: poor processing of social information, limited fear response
- Oppositional temperament
- Frequent parent-child conflict which the child wins
- Social: early maternal rejection, childhood maltreatment, harsh & inconsistent discipline, parental marital discord
Treatment of externalizing disorders
Interventions need to address the family and social context.
Cognitive behavioral parental education can teach parents:
- To regulate their own emotions
- increase positive interactions with their children
- establish appropriate rules
- consistently implement consequences for inappropriate behavior
Psychosocial interventions can teach youngsters:
- assertiveness
- anger management techniques
- skills in empathy, communication, social relationships and problem solving
- Adult mentors can demonstrate empathy, warmth and acceptance.
Neurodevelopmental Disorders
Impaired developments of the brain and central nervous system.
Include:
- Tics & Tourettes disorder
- Attention-deficit/hyperactivity Disorder
- Autism Spectrum Disorders
- Intellectual & learning disorders

Tics and Tourettes
- involuntary repetitive movements or vocalizations.
- may persist into adulthood
- 4 x more common in males
- Tourettes is characterized by multiple motor tics and one or more vocal tics. May include coprolalia -having a strong urge to say inappropriate things or swear
- Appear to have a genetic base
- Prenatal factors include maternal alcohol and drug use and underweight mother during gestation
- Highly comorbid with OCD
- Habit reversal can help with the tics

Attention deficit/Hyperactivity disorder
- Twice as common in males
- may persist into adulthood
- The child cannot pay attention and/or behaves in an impulsive, hyperactive way
- Becomes apparent when the child goes to school.
- for diagnosis, symptoms need to
- appear before age 12
- persist for at least 6 months
- interfere with social or academic functioning
- Highly diagnosed and prescribed medication
- Highly hereditable disorder – possible overlapping genetically with bipolar & schizophrenia
- neuroimaging show that the frontal cortex, cerebellum and parietal lobes may be underdeveloped in children with ADHD
- There may be functional abnormalities in the frontal lobes associated with inhibition of responses and attention.
- Neurotransmitters such as dopamine and GABA my be underactive and therefore reduce signal to and from the frontal lobes
- Other biological factors that have been implicated include:
- prematurity, perinatal oxygen deprivation, low birth weight, exposure to pollution, viral infections, meningitis & encephalitis and maternal smoking and drug and alcohol use.
- Also associated with family stress, marital discord, poverty, foster care, parental mental disorders
- May be associated with acting out due to depression, low self esteem and rebelliousness
- Treatment is though Ritalin, but behavioral and psychosocial treatments have been shown to be effective too.

Autism spectrum disorder ASD
significant impairment in social communication skills, and stereotyped interests and behaviors
- Along a spectrum from mild to severe
- increasing prevalence
- 5x more common in boys than girls
- Characterized by:
- Deficits in social communication and interaction:
- lack of reciprocity and acknowledgement of others,
- atypical non verbal communication
- no eye contact
- no meaningful gestures and facial expressions
- treating people as if they were objects
- poor social boundaries
- Difficulties in developing and maintaining relationships lack of interest in others, lack of social play, not recognizing other people’s identity and emotions
- Repetitive behavior or restricted interests or activities involving:
- repetitive movement, speech or use of objects eg spinning, flapping, or stacking or spinning objects, repetitive echoing or what is said (echolalia) and one-sided conversations
- Intense focus on rituals or routines and strong resistance to change
- Intense fixations or restricted interests
- atypical sensory reactivity – either underreactive or overreactive
- Deficits in social communication and interaction:
These symptoms can be very impairing.
Almost half of all people diagnosed with ASD are high functioning.
But about a third have significant cognitive impairment.
Some children only start showing symptoms when they are a year or older, and these children, who have regressive autism are often more severely affected.
Etiology of ASD
Intense early intervention has sometimes reversed or eliminated the progression of the disorder.
This makes early diagnosis very important.
Autistic traits do seem to be somewhat hereditable, and there are many neurological findings such as
- unusual brain metabolism
- high levels of serotonin
- elevated response in the amygdala to human faces
- patchy areas of disrupted neuronal development in the frontal and temporal cortex
- possibly associated with neonatal exposure to toxins such as pesticides and heavy metals.

Intellectual Disability ID
Significant limitations in intellectual functioning and adaptive behaviors
- IQ of 70 or less. mild: 50 – 70, moderate 35 – 55, severe 20 – 40 and profound 20 – 25
- deficiencies in adaptive behavior: self-care, health care, ability to life and work independently
With support and intervention, people with ID can make cognitive and social gains and live satisfying lives.
Mild ID may be idiopathic. More severe ID may be due to genetics, brain abnormalities or brain injury. eg: Fragile X syndrome, Down syndrome, exposure to infections such as Tuberculosis, iodine deficiency during pregnancy and many other conditions may cause ID.
Learning disorders
A person with average or above intellect is not learning at a pace that matches their true capacity.
- Dyslexia = reading difficulties
- Dyscalculia = difficulties in understanding math
- Dysgraphia = writing difficulties
- often comorbid with ADHD
- 2x as frequently a problem for boys
- May have lifelong difficulties
- Strong genetic component
In general, children benefit from early and intensive interventions. For severe ID & ASD, this may begin in infancy
For ADHD, LD, mild ID or mild SD, this support may be through the school setting
Parental involvement is an integral part of intervention. Many people need ongoing support through adulthood.

