Anxiety, OCD & more
We need to know the symptoms from the tutorial letters and also remember to learn the duration of the symptoms needed for a positive diagnosis. The biological and psychological dimensions are particularly important to remember for exams.
- 7 Anxiety disorders:
- phobias
- agoraphobia
- specifice phobias
- social anxiety disorder
- panic disorder
- generalized anxiety disorder
- separation anxiety disorder
- selective mutism
- phobias
- Obsessive Compulsive:
- OCD
- Body Dysmorphic disorder
- hair-pulling disorder
- skin-picking disorder
Diagnostic Duration chart
| Phobias | 6 months |
| Panic Disorder | At least a month |
| selective mutism | At least a month |
| separation anxiety disorder | 1 month for kids, 6 for adults |
| GAD | At least 6 months, most days for more than an hour. |
| OCD | At least a month for more than an hour every day |
Anxiety from a multi path perspective
Anxiety disorder: Unfounded anxiety that interferes with functioning and produces distress and life-impairment.
Symptoms of Anxiety
- Affective or emotional symptoms:
- fear
- watchful
- dread
- terror.
- Cognitive symptoms
- from worry to panic.
- Harm may be anticipated,
- danger may be exaggerated
- severe forms can bring a conviction of impending doom (the end of the world or death).
- Concentration problems
- fears of losing control and dying
- a sense of unreality
- hyper vigilance
- Behavioural symptoms
- avoidance behaviour,
- freezing,
- clinging,
- dependent
- agitated behaviour.
- Somatic symptoms are changes in a person’s physiological or biological reactions.
- increased heart rate and perspiration,
- elevated blood pressure,
- tense muscles,
- goose bumps,
- shallow breathing,
- mouth dryness,
- cold hands and feet,
- diarrhoea,
- frequent urination,
- dilated pupils,
- light-headedness, faintness
- indigestion
Biological causes of anxiety
- The symptoms may because of medicines or other physical causes:
- asthma meds, caffeine,
- hyperthyroidism, cardiac arrhythmias
- Overactive Fear circuitry in the brain
- Amygdala triggers the hypothalamic-pituitary-adrenal (HPA) axis
- And also the hippocampus & prefrontal cortex
- Genetics
- On their own they are not sufficient to explain phobias, panic disorder etc..
- Some genetic variations correlate with less serotonin and also with higher anxiety amongst people with high childhood stress and low maternal support.
Psychological causes for anxiety
- negative appraisal : interpreting ambiguous events as threatening
- anxiety sensitivity: Interpreting physical arousal as a sign of danger
- Feeling a lack of control over the situation
Social & Sociocultural Dimensions to anxiety
- Unsafe environments eg poverty & high crime
- Traumatic events
- Gender (more women than men)
- Some cultures eg North American white report more anxiety than others
Phobias
= strong, persistent & unwarranted fear of a specific thing or situation
3 Categories:
- social anxiety disorder SAD
- Intense fear of being looked at or being embarrassed or humiliated. Usually around public speaking or meeting new people.
- specific phobia
- Fear or panic about specific things/situations eg mice, spiders, needles
- agoraphobia
- Anxiety or fear in situations that cannot be escaped. So situations are avoided or may cause panic.
- The following situations (at least two or more) are feared and avoided:
- being in a crowd of people or standing in line,
- using public transportation, or
- being in open spaces
- or in enclosed places or
- being outside of the home alone.
Etiology of phobias
Biological dimension
- All phobias show moderate genetic contribution (heritability of 30%)
- More active amygdala
- Some phobias, eg of snakes, may be semi-innately predisposed
Psychological dimension
- Fear conditioning
- phobias can be created
- and often the result of a frightening experience
- Observational learning/modeling
- learn from others displaying fear
- negative informational effects
- In other words, people develop fears because they are told scary things about a thing or situation
- cognitive processes
- catastrophic thoughts and cognitive distortions can cause phobias to develop and sustain themselves.
Social Dimension
- Overprotective parents
- Parents who don’t support their children’s independence and confidence. So the children don’t develop emotional regulation and coping skills
- negative family interactions and stress
- Being bullied
Sociocultural Dimension
- Females more likely to have phobias about critters, and a stronger disgust response
- Social anxiety is not gender differentiated, but more common in collectivist cultures that use shame as a way of disciplining their children eg: Chinese and Arab societies
Treatments
- Biological: benzodiazepines and SSRIs (Selective Serotonin Re-uptake inhibitors)
- Psychological: CBT:
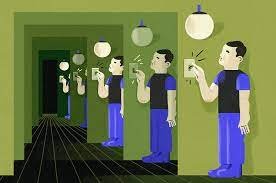
- exposure therapy: Gradual and increasing exposure without inducing panic
- systematic desensitization: Conscious physical relaxation while visualizing the situation or thing that triggers fear
- cognitive restructuring: identifying and changing unrealistic negative thoughts to more helpful ones
- modeling therapy: observing a model remaining calm in the situation or with the thing.
Panic Disorders
Recurrent and unexpected intense attacks of fear or terror
Along with fear of having another attack and what may happen during an attack (May feel like a heart attack, for example)
and/or changes in behavior to avoid having another panic attack.
For a month or more for a positive diagnosis of panic disorder
Two types of panic attacks are described in the DSM-5 classification system:
Expected panic attacks are attacks that have an obvious cue or trigger
Unexpected panic attacks (e.g., when relaxing)
Symptoms of Panic Attacks
A panic attack is characterised by a discrete period of intense fear or intense discomfort and is accompanied by at least four or more of the following symptoms:
- (1) palpitations, pounding heart or accelerated heart rate
- (2) sweating
- (3) trembling or shaking
- (4) sensations of shortness of breath or smothering
- (5) feelings of choking
- (6) chest pain or discomfort
- (7) nausea or abdominal distress
- (8) feeling dizzy, unsteady, lightheaded, or faint
- (9) chills or heat sensations
- (10) paraesthesia’s (numbness or tingling sensations)
- (11) derealisation (feelings of unreality) or depersonalisation (being detached from oneself)
- (12) fear of losing control or “going crazy”
- (13) fear of dying.
Biological Dimension
- Modest genetic influence 32% heritability
- Overactive fear network (amygdala)
- Serotonin and GABA less available
Psychological Dimension
- Catastrophic thought eg: “I will die.”
- sensitive to anxiety and physiological vigilance
- conditioning
Social Dimension
- Stressful and anxiety provoking social environment
- Separation or loss
- Being bullied
Sociocultural Dimension
- More common in women
- Varied cultural expression
- More common in some cultures than others
Treatment of PD
The primary treatments are medication and CBT.
Meds include benzodiazepines, beta-blockers and anti-depressants, but relapses once the person comes off the medications are high. Influences the amygdala
CBT is very effective in treating Panic Disorder. Influences the prefrontal cortex and hippocampus
- Increases self-efficacy as client get control of the disorder themselves
- Involves the extinction of the fear associated with both
- Internal bodily sensations:
- heart rate
- sweating
- dizziness
- breathlessness
- Frightening situations
- eg crowds, enclosed spaces etc
- Internal bodily sensations:
- Involves the following steps:
- Educate about PD and correct misconceptions
- Identify and correct catastrophic thinking
- Teaching to self-induce the sensations (aka physiological symptoms) associated with panic in order to extinguish the conditioned response of panic in response to these internal sensations.
- Encouraging the client to sit with the symptoms without responding to them
- Teach coping statements: “I can handle this.”
- Teach the client to identify potential triggers before the panic starts.
Generalized Anxiety Disorder GAD
Characterized by persistent high levels of anxiety and excessive and difficult to control worry, accompanied by physical symptoms
Symptoms must be present for most days for 6 months and cause distress and difficulty functioning in everyday life.
Symptoms of GAD
The anxiety and worry are associated with three or more of the following six symptoms:
- (1) restlessness or feeling keyed up or on edge
- (2) being easily fatigued
- (3) difficulty concentrating or going blank
- (4) irritability
- (5) muscle tension
- (6) sleep disturbance.
The anxiety, worry or physical symptoms cause clinical significant distress and/or impairment in social, occupational or other important areas of functioning
Etiology
Biological Dimension
- Heritability small but significant: Gene expression of neurotransmitter abnormalities or overactivity of brain regions associated with anxiety
- GAD involves a disruption of the prefrontal cortex which modulates our response to threats. Greater activation than in controls
Psychological Dimension
- Dysfunctional thoughts and beliefs
- Lower threshold for uncertainty
- Assume that worry is a strategy to deal with problems
- And that it prevents negative outcomes from occurring
- Negative schemas paint many ambiguous, neutral or even positive situations as threatening
- May also involve worrying about worrying.
Social & Sociocultural Dimensions
- Affect twice as many women as men
- Anxious mothers seem to increase the chances that their children will have GAD.
- Being bullied
- Stressors such as poverty, prejudice and discrimination (This may by why GAD is high amongst African-Americans and Latino/Hispanic Americans
Treatment of GAD
- Benzodiazepines (nastily addictive) and antidepressants
- CBT is very effective
- identify worrisome thoughts
- identify which worries are useful and which not
- evaluate beliefs and evidence
- develop self control skills to monitor and challenge irrational thoughts and replace with more positive ones
- use muscle relaxation
Obsessive Compulsive Disorder
Obsessions are persistent anxiety-provoking thoughts and images.
Compulsions are an overwhelming urge to do something to counteract anxiety or ward off a dreaded event.
For a diagnosis, these symptoms should take up at least an hour a day and cause significant distress or impairment in life activities.
Onset is in adolescence or early adulthood – 25% by age 14. Equally common in both men and women.
Compulsions involve repetitive actions eg hand washing. Obsessions and compulsions offend occur together, although they can also be separate.
Compulsions often serve to neutralize obsessions.
The compulsion feels involuntary, irrational and not in character to the person with OCD, but resisting it causes more and more anxiety.
Frequent comorbidity with depression and substance abuse.
About a quarter of people report some symptoms without having the disorder.
Common themes:
- Contamination
- errors or uncertainty
- unwanted impulses
- orderliness
Hoarding Disorder
Hoarding disorder is diagnosed when there is 1. an inability to discard items regardless of their value,
2. a perceived need for items and distress at the thought of getting rid of them and
3. an accumulation of items
that results in distress or impairment in life activities.
Prevalence is quite high 2 – 5% of adults in the US.
Body Dysmorphic Disorder
A preoccupation with a perceived physical defect, repetitive behaviors and comparing one’s appearance to others, and significant distress or impairment in life activities.
Often underdiagnosed. Some people recognize that their beliefs are untrue, but others have strong delusions about their bodies.
Some people have a lot of cosmetic surgery because of BDD.
Up to 13% of people in psychiatric hospitals, and 15 % of people who consult dermatologists. High comorbidity with anxiety disorders especially social anxiety
Trichotillomania Hair-Pulling Disorder

Recurrent and compulsive hairpulling. 10 x greater in women
Excoriation (Skin-picking) Disorder

Compulsive skin picking causing significant distress or impairment with repeated unsuccessful attempts to stop.
Often comorbid with BDD and trichotillomania.
Etiology of OCD & related disorders
OCD may involve distinct disorders with different triggers and causes. We are still not quite sure what causes OCD.
Biological Dimension
- Strong heredity
- Increased activity in the orbitofrontal cortex
- The orbitofrontal cortex alerts the brain that something is wrong. So when it is hyperactive, it feels like something is horribly wrong.
- Lower activity in the caudate nuclei
- Subgroups differ in genetics and biological markers
- Reduced availability of serotonin and glutamate.
- OCD responds specifically to SSRI’s and not to other kinds of anti-anxiety meds.
Psychological Dimension
- Lack of trust in own performance
- Impulse control conflicts
- compulsive behaviors reduce anxiety, and because they reduce anxiety, they create compulsions through conditioning
- cognitive disorders
- exaggerated estimates regarding the probability of harm
- control seen as essential
- intolerance of uncertainty
- Search for evidence that they may have failed to perform rituals correctly – disconfirmatory bias
- hoarders may feel responsible towards the items or that they are extensions of themselves.
Social and sociocultural dimensions
- Controlling, over-critical parenting
- Low parental warmth
- Discouragement of autonomy in the child
- These factors may give rise to maladaptive beliefs relating to personal responsibility.
- More common among white Americans
- And people who are divorced, seperated or unemployed
Treatment of OCD & related disorders
- Only about 60% of people with OCD respond to SSRI’s and may only respond partially.
- Behavioral treatments combine
- exposure: continued actual/imagined exposure to anxiety provoking situations, either gradual or flooding with the most stressful scenario
- response prevention
- Involves education about OCD, exposure and response prevention
- Development of an exposure hierarchy – ranking from least to most feared
- Exposure until anxiety goes down
- Prevention of compulsive rituals being acted out
- About 70% success-rate in OCD, and good results in related disorders.
- However many hoarders leave treatment because they don’t want to let go of their stuff.