Depressive and bipolar disorders are both mood disorders and are associated with an increased risk of suicide.
How do we distinguish a normal range of negative or labile moods from a disorder?
- The moods affect the person’s wellbeing and ability to function
- They continue for days, weeks or months
- They often occur for no reason
- There are extreme reactions that are not explained by circumstances.
Symptoms of Depression
Depression
A mood state characterized by sadness or despair, feelings of worthlessness and withdrawal from others
Essentials of Understanding Abnormal Behavior – Sue
Cognition
- Pessimism
- guilt
- difficulty concentrating
- negative thoughts and rumination (which can make things worse)
- suicidal ideation (possibly feeling like a burden, unwanted etc…)
Behavioral
- social withdrawal
- crying
- low energy, lethargy
- lowered productivity
- agitation
- poor hygiene
Physiological
- appetite and weight changes
- sleep disturbances
- aches and pains. In some cultural groups, these are the main symptoms reported
- loss of sex drive
Symptoms of mania

EXALTATION (2014)
In bipolar disorder, people swing between mania and depression.
Mania
Pronounced mood change: Extremely exaggerated activity levels and emotionality that impair normal functioning. giddiness, euphoria or hostility, irritation and agitation.
Mania may involve psychosis and require hospitalization.
Easily apparent to others
Hypomania
Milder form of mania: More energy and a feeling of self-importance and expansiveness or irritation. Easily distracted, creative, having many ideas. Impulsivity, poor judgement and risk taking. The person may talk excessively and take over conversations.
May only be noticeable to people who know the person, and the person may still be able to function in everyday life.
Mood
- elevated mood
- extreme confidence
- grandiosity
- irritability
- hostility (The symptoms may be quite difficult for others to tolerate as well, so may get into conflict as a result.)
- emotional lability (mood swings)
Cognition
- Disorientation
- racing thoughts, often goal oriented in hypomania.
- flight of ideas: change topics, get distracted with new thoughts, and make irrelevant or illogical comments
- decreased focus and attention, may fail to recognize that their behaviour is inappropriate
- creativity
- poor judgement
- pressured speech (rapid, loud, difficult to understand)
Behavioral
- overactivity
- rapid or incoherent speech
- impulsivity – uncontrolled spending, changing jobs or moving.
- risk-taking behaviors – such as drug use, promiscuity, driving too fast
- In extreme mania the person may rant and rave, move constantly and experience psychotic symptoms such as hallucinations and delusions, becoming a danger to themselves and others.
Physiological
- high levels of arousal
- decreased sleep – may go for days without sleep
- increased sex drive
Evaluating symptoms
This can be quite tricky, because people may have differing symptoms, and there may be mixed features:
- Some depressed people may be irritated and agitated, and unable to sleep, or have racing thoughts
- Some people in mania or hypomania may be crying and talking of suicide
For these reasons clinicians complete a checklist with patients, covering:
- behavioral symptoms
- mood, cognition and physiological symptoms
- frequency
- duration
- seasonality
- intensity (mild, moderate or severe)
- Other factors that may cause symptoms:
- thyroid imbalances
- use of alcohol and drugs (illegal and prescription)
It is important to distinguish between depression and bipolar because the treatments are different. A person may also need to be reassessed as moving from one state to the other can happen as well.
Depressive Disorders
8 types of Depressive Disorders:
- Major depressive Disorder
- Persistent Depressive Disorder (Dysthymia)
- Premenstrual Dysmorphic disorder
- Disruptive Mood Dysregulation Disorder
- Substance/medication Induced Depressive Disorder
- Depressive Disorder due to another medical condition
- Other Specified
- Unspecified
Key Vocabulary
Apathy
lack of motivation and drive
Anhedonia
Unable to experience happiness or pleasure
Lethargy
Lack of energy
Self-denigration
Putting yourself down.
Catatonia
Abnormality of movement and behaviour arising from a disturbed mental state (typically schizophrenia).
It may involve repetitive or purposeless overactivity, or catalepsy, resistance to passive movement, and negativism.
melancholia
Deep sadness
Rumination
Rumination is the tendency to focus passively and repetitively on one’s problems without taking action to relieve them.
Unipolar Disorder
Depressive disorder
Major Depressive Disorder
To get a diagnosis of MDD – Major depressive disorder, a person:
- must have had symptoms at least once for 2 weeks. (a major depressive episode)
- must not have had any symptoms of mania or hypomania
- A major depressive episode has
- severely depressive symptoms
- that negatively affect functioning
- nearly every day
- for most of the day
- for at least 2 weeks
- It involves a consistent pattern of:
- depressed mood, feelings of sadness or emptiness
- loss of interest or pleasure in previously enjoyed activities
- In addition at least 4 additional changes in functioning including
- significant changes in weight or appetite
- sleep pattern changes
- restlessness/sluggishness
- low energy
- feeling guilt or worthlessness
- persistent difficulty with concentration or decision-making
- suicidal behaviors or recurrent thoughts of death or suicide
The lifetime prevalence is 14 to 19%, and it is much more common in women.
Major depressive disorder can begin at any age, but most usually occurs in the late 20’s

Major Depressive Disorder and Suicide Risk
Suicide is a risk for anyone with MDD. People with MDD who feel hopeless or impulsive (especially if they feel rejected by their community or family) may act on suicidal impulses, especially if they are under the influence of drugs or alcohol.
Nearly a third of people with MDD also have a substance-use disorder, which increases suicide risk.
People with chronic long term depression or who develop suicide in response to grief also have an increased risk of suicide.
| Major Depressive Disorder | Grief |
| persistently depressed mood, inability to anticipate happiness or pleasure | Feeling emptiness & loss |
| Depressed mood is persistent and not tied to specific thoughts. | Occurs in waves, and diminishes over time. Connected with thoughts and reminders of the person who has been lost. |
| Pervasive unhappiness | Pain as well as positive emotions and humor |
| Self-criticism and pessimism | Thoughts of the person who has been lost |
| Feelings of worthlessness and self loathing | self esteem usually preserved. Self-derogatory ideation will be about the deceased. |
| Thoughts of ending your own life because of feeling worthless, undeserving and or unable to cope. | Thoughts of the deceased and possibly joining them |
Persistent Depressive Disorder (Dysthymia)
Chronic depressive symptoms present for most of the day for more than half the time over a 2 year or longer period. (with no more than 2 months symptom free).
At least 2 of the following symptoms:
- feelings of hopelessness
- low self esteem
- poor appetite/overeating
- low energy or fatigue
- difficulty concentrating or making decisions
- sleeping too much or too little
Some people have this as a life-long pervasive disorder with poor response to treatment.
Premenstrual Dysmorphic disorder
Involves serious symptoms of depression, irritability and tension before menstruation. Very similar to premenstrual syndrome, but cause much greater distress and interfere with the woman’s ability to function.
The diagnosis requires at least 5 symptoms, and at least one of them must involve:
- significantly depressed mood
- mood swings
- anger
- anxiety
- tension
- irritability
- increased interpersonal conflict
Other possible symptoms:
- difficulty concentrating
- social withdrawal
- lack of energy
- food cravings or overeating
- insomnia or excessive sleepiness
- feeling overwhelmed
- bloating, weight gain or breast tenderness
Disruptive Mood Dysregulation Disorder
Only added to the DSM 5 in 2013.
Mental disorder in children and adolescents (age 6 to 18, must start before age 10) with persistently irritable or angry mood and frequent temper outbursts that are disproportionate to the situation and significantly more severe than the typical reaction of same-aged peers.
Outbursts 3 or more times per week and in multiple settings.
More prevalent amongst boys, associated with autism
Prevalence of depressive disorders
Lifelong prevalence of 19% in the US.
Depression is the second leading cause of disability worldwide.
For many people depression is a chronic condition, and about 15% of people fail to improve with medication – it is possible that some of these people may have bipolar disorder that has not been diagnosed.
Etiology of depressive disorders
Environmental factors more influential in childhood depression.
Hereditary factors in adolescence and adulthood. Mid-adolescence is when genetic conditions and predispositions often make themselves known.
Biological dimension
- Neurotransmitters: low levels of serotonin, norepinephrine and dopamine are associated with depression
- Heredity: Depression does run in families and it does so often according to the type of depressive disorder. And the incidence is higher amongst female than male twins. The short allele of the serotonin transporter gene 5-HTTLPR is associated with depression – especially if there is also childhood stress and trauma. So it is a mix of gene expression and environmental triggers.
- Cortisol and stress: Dysregulation and overactivity of the HPA axis – the hypothalamic-pituitary-adrenal axis and overproduction of cortisol seem to cause depressive symptoms in adolescents and in adults. Again, childhood trauma and stress seem to be correlated with high cortisol levels later in life, possibly due to gene expression. 5-HTTLP has been shown to be implicated.
- Brain changes: Decreased brain activity, changes in brain anatomy. 5-HTTLP comes up once again as correlated with stress-induced changes in the hippocampus, which regulates stress and emotions. , Reduced neuroplasticity, including reduced neurogenesis in the hippocampus and the cortical synapses.
- Circadian rhythms: Some people get seasonal depression in winter. Melatonin being disrupted is implicated in seasonal and non-seasonal depression.
- Insomnia doubles the risk of developing depression
Psychological Dimension
- Behavioral explanations: Insufficient social reinforcement.
- Social loss of connection such as getting dismissed, ending a relationship, bereavement, the end of a friendship, business failure etc etc.
- General stressful circumstances also threaten access to social reinforcement and connection.
- A positive feedback loop: As life gets tough, negative self talk and expectations as well as a loss of self-confidence can trigger social withdrawal. Social disconnection in turn, triggers depression. Which makes it harder to get ahead.
- Cognitive explanations: Some people see depression as disturbed thinking rather than disturbed mood.
- It is correlated with pessimism
- and negative perspectives.
- Global thinking, generalizing from a single negative experience that becomes engrained.
- This then causes more hopelessness and pessimism
- no positives can be seen or believed to be real.
- Rumination rather than problem-solving
- co-rumination is constantly talking over the negatives and stressors, and can also increase risk of depression
- Learned helplessness attributional style:
- Attributional style is how we attribute explanations to events.
- Learned helplessness is an attributional style in which we believe that we don’t control what happens to us.
- The attributional style associated with depression is:
- negative
- internal : because of me
- global : always and in all situations (space)
- stable : This is going to go on forever. (time)
- Once the world and the self is viewed this way, hopelessness, helplessness and overwhelm can easily lead to depression, and this way of thinking can become habitual. A more helpful and true to reality attributional style would be more
- external (it’s not personal),
- unstable, (This is just happening here and does not reflect the nature of reality everywhere)
- and specific (this too will pass).
- Negative attribution styles are in and of themselves deeply harmful to people. They can become a deeply engrained habit, that can make a person feel like life is terrible.
- Negative self-concept, self criticism, self-contempt, self-blame as cognitive patterns can give rise to lifelong deep personal suffering and to depression and other disorders.
Social Dimension

- Severe acute stress : like losing a loved one or being seriously ill often precedes the start of a major depressive episode.
- Chronic stress: Less associated, but still significant is chronic stress. Jobs with high stress, social isolation and lack of access to support seem to have the highest correlation with depression.
- When a person has already had a depressive episode, more stress can trigger more depression.
- Childhood maltreatment is a very significant predictor of future depression.
- Social rejection is another specific trigger for depression, most especially when it is personally targeted.
- Stress generation: And of course depression makes a person quite difficult to be around sometimes. It can may initiate and sustain substance abuse problems, being argumentative and negative, so that the person then gets less social support and is more in danger.
Sociocultural dimension
- Culture:
- Culture affects how people conceptualize, experience and describe their depression
- feeling “heartbroken”, “nerves and headaches”, “out of balance”, “aching and tired” etc…
- and it affects risks and outcomes such as effectiveness of different treatments, and suicide risk.
- it also affects the treatment choices and the therapeutic relationship.
- Culture affects how people conceptualize, experience and describe their depression
- race and ethnicity: The experience of discrimination is correlated with depression
- sexual orientation: Prejudice and discrimination are again important causes for depression amongst LGBQT+ people. Families and communities that are unwelcoming and unsafe to come out of the closet to are major stressors.
- Gender: A strong correlation between being female and being prone to depression. Sexual abuse also correlates.
Treatment for depression
Biomedical
1. Medication
Medication works by increasing the availability of:
- Norepinephrine
- serotonin (SSRI’s such as prozac)
- dopamine
Many many people take antidepressants, and often long term, but their efficacy in mild to moderate depression is dubious or none.
They are of benefit in severe depression.
(Risk of increased suicidality in people younger than 25.)
Exercise and omega 3 supplements seem to help more.
2. Circadian-related treatments
Some treatments work by resetting the body clock’s sleep-wake cycle and exposing people to more natural dawn to dusk light patterns.
This seems to be effective even for some people with depression that does not at first seem to be seasonally affected.
3. Brain stimulated therapies
- Electroconvulsive therapy (ECT) – alarming memory loss and confusion as a side effect
- vagus nerve stimulation – new therapy – has had some profound and sustained positive outcomes for some people.
- transcranial magnetic stimulation
May be prescribed for severe or treatment resistant depression.
Psychological and Behavioral Treatments
Psychotherapy and behavioral treatments have better and more long lasting results than medication for depression.
- Behavioral activation: Based on operant conditioning to help people participate in social and fun activities.
- Interpersonal psychotherapy: helping people work through current interpersonal problems, focussing on relationships. Proven to be effacious.
- CBT: Changing negative cognitions to positive
- mindfulness-based cognitive therapy: Learning to be present and calm rather than to assess and label thoughts and feelings, so that ruminative negative thought patterns and habits are broken.
Bipolar disorders
Diagnosis and classification
Because the treatments are different, and misdiagnosis can result in ineffective treatment, it is very important to distinguish bipolar for depressive disorders. Careful and thorough questioning of the client is needed.
The depressive symptoms are more disruptive than the manic ones, usually.
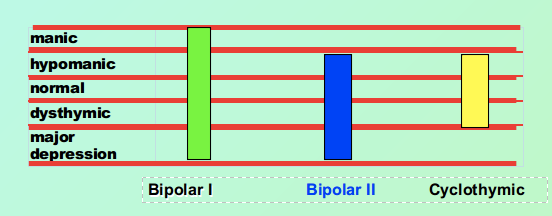
There are 3 types: bipolar 1, bipolar 2 and cyclothymic disorder.
DSM Criteria
Hypomanic/manic episode: Definite observable change in behavior, most of the day, nearly every day, involving a consistently elevated, expansive or irritable mood and unusual increases in energy or goal-directed activity.
- Grandiosity, exaggerated self-esteem & self-importance
- Less need for sleep
- talkative, pressured speech
- racing thoughts, frequent topic changes
- distractable
- work, sexual & physical activity goes up
- impulsive
Hypomanic: for at least 4 days
Manic: At least 1 week + requires hospitalization or impaired functioning. Possible psychosis
Bipolar I, bipolar II and cyclothymic
There are three different types of bipolar. The essential difference between them is the intensity and range of the moods.
Features and conditions of Bipolar Disorder
Mixed features: Symptoms of mania while depressed, or depression while manic or hypomanic.
Rapid Cycling: 4 or more mood episodes a year
common comorbidities: anxiety disorder (especially panic attacks) 75%, ADHD, eating disorders, substance abuse and suicidal ideation with increased risk of suicide.
Biological Dimension
- complex genetic basis
- circadian rhythm abnormalities
- associated with elevated glutamate neurotransmission in the brain
- In some cases triggered by traumatic brain injury
- common genetic vulnerabilities with schizophrenia
Suicide
Alright. I am now behind, and the following section is going to be incredibly sketchy and not thorough. Please visit the textbook and ensure that you don’t rely on this study aid for a full overview.
Key points
Up to 90% of all people who have suicidal ideation have a mental illness. And mental illness is associated with a risk of suicide.
Suicide is the 10th leading cause of death in the US, and second leading cause of death amongst college students. The most at risk populations are children/adolescents and the elderly
Not everyone who commits suicide wants to die as such. Some simply want to end their pain.
1 in 25 suicide attempts end in death.
Common characteristics:
- Belief things will never get better – suicide is the only solution
- Desire to escape painful thoughts and feelings
- Triggering events:
- intense fights/conflict
- depression
- hopelessness
- anger
- guilt
- shame
- Feeling unable to make things better (failure, worthlessness, hopelessness)
- ambivalence about suicide
- communicate the intent through verbal or behavioral cues
Suicide prevention
- Reawaken and reinforce the desire to live
- Expand point of view so that suicide no longer looks like the only option
- enhance social connection and support
- help the person develop more coping skills